Key Takeaways
- Individual glucose responses vary significantly based on insulin sensitivity, gut microbiome, sleep, stress, and meal timing, making your most effective method of improving metabolism different from someone else’s.
- Insulin resistance can cause your body to store more fat and make it harder to burn it.
- Strategic adjustments like portion control, food order changes, and activity timing based on CGM data enable personalized fat loss without restrictive dieting.
that {{mid-cta}}
You're tracking calories, swapping refined carbs for whole grains, and cutting back on sweets, but your weight-loss efforts have hit a plateau. Sound familiar? The issue might not be your effort, calories, or even the types of foods you’re eating. It might be how your body is responding to that food.
Continuous glucose monitoring (CGM) helps you better understand how your body responds to the food you eat. This data can reveal patterns that indicate whether specific foods may be triggering prolonged insulin exposure, which can block fat loss. By identifying these weight-loss-blocking foods through data rather than guesswork, you can make changes to your diet and habits that actually move the needle toward improving your metabolic health and achieving your goals, without guessing or unnecessarily cutting out the foods you love.
In this article, you’ll learn why some foods block weight loss, insulin’s role in fat storage and metabolism, and how to use a CGM to identify and experiment with foods to support your metabolic health goals.
Why Some Foods Block Weight Loss Regardless of Calories
.jpg)
While much traditional weight-loss advice follows a “calories in, calories out” approach, this treats all the energy from food as equal. But we know that 200 calories from a piece of cake has a much different effect on your metabolism than 200 calories from a piece of chicken or a dish with leafy greens, beans, and lean protein.
When you eat, your pancreas secretes insulin to help move glucose from your bloodstream into your cells for energy. What isn’t needed immediately is stored in the liver and muscles for short-term use, and once those are full, the rest is stored for long-term energy as fat.
Consistently eating simple-sugar, high-carbohydrate foods increases the amount of insulin circulating in your system, which not only promotes fat storage if that energy can’t be used quickly enough, but can also inhibit fat breakdown, making it harder to lose weight.1 While too many calories from any nutrient, including fat and protein, can lead to increased fat storage, a higher percentage of added sugars in your diet increases the likelihood of elevated insulin levels.1
The timing of what you eat also affects how likely it is to be used for energy or stored as fat. One small study found that, compared to eating a dinner at 6 pm, a late dinner at 10 pm resulted in an 18 percent greater glucose peak and a higher, extended insulin peak, creating an anabolic state that favors fat storage over energy expenditure.2
How Continuous Glucose Monitoring Can Reveal Hidden Glucose Spikes
.png)
Traditional food tracking apps can tell you how many calories or carbohydrates are in your meals, but they can’t tell you how your body responds to those carbohydrates. Given the variability in individual metabolism as well as your activity, sleep, and meal timing, understanding how your body responds can help you make intentional and impactful changes.
Ideally, your glucose levels should rise gradually after eating, then fall gradually, with your insulin levels rising and falling along with it. Because protein and fat slow down digestion, you may even see a “biphasic” curve, where your blood glucose rises, then falls slightly, then rises again as your body slowly digests and absorbs the carbohydrates you’ve eaten.
While we can predict with some accuracy that certain foods will cause a larger, longer rise in glucose and insulin (large meals of refined carbs or sugar-sweetened drinks, for example), researchers have found that variables like your unique gut microbiome, specific sensitivity to insulin, and factors like food order or meal timing also play a large role in a person’s unique post-meal (post-parandial) glucose response.3
By monitoring your glucose levels and how various foods, food combinations, movement, sleep, stress, and timings play a role, you can adapt your habits and meals to support stable glucose levels that keep your body energized while reducing the amount of fat your body stores.
Understanding Insulin Resistance and Weight Loss Hurdles
Under normal conditions, your body is well-equipped to digest, absorb, and metabolize carbohydrates, efficiently turning them into usable energy for your cells. But when your cells become responsive to insulin’s signals to transport glucose from the bloodstream into your cells, insulin resistance may be to blame.
Your pancreas has to pump out more and more insulin to help trigger the cells' uptake of glucose, which leads to higher baseline insulin levels, making fat loss significantly harder to achieve.
When insulin resistance is at play, you’ll see a much greater response to even moderate or lower carbohydrate foods, which creates a cycle of higher glucose, more insulin, more resistance, and more fat storage.4In this case, even foods that work well for others may become weight loss blockers until insulin resistance is reversed. A CGM can help you identify insulin resistance even before routine lab work may spot a concern.
How to Spot Weight Loss Blocking Foods with CGM Data
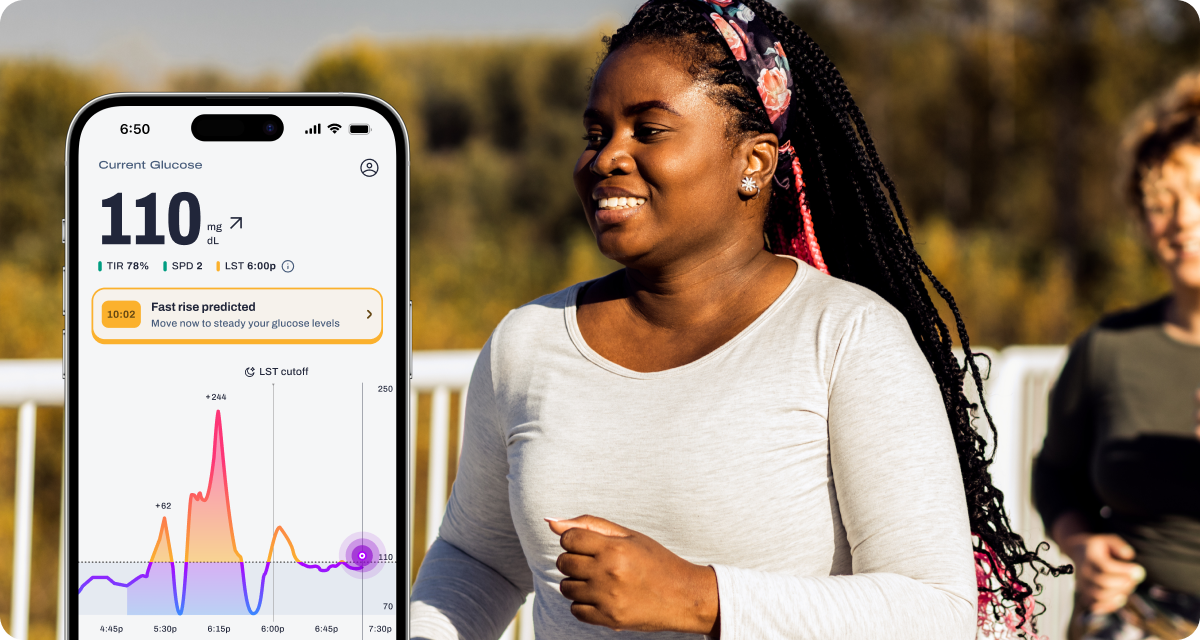
Using a CGM to analyze your peak glucose level, the time to reach that peak, the time your glucose spends above the recommended range, and the frequency of your glucose spikes can help you identify which foods may be making it harder to burn fat.
How High Are Your Glucose Level Peaks?
After eating, your glucose should rise gradually, ideally staying below 140 mg/dL even at its highest point about 1-2 hours after eating, most of the time, if you do not have diabetes. Consistent peaks above 140 mg/dL signal that your body is producing excess insulin to handle that food, increasing fat storage potential.5
How Long Does It Take for Glucose to Peak?
When you’re eating a meal or snack that includes carbohydrates, protein, and fat, you can expect a slower rise in glucose levels as the protein and fat help to slow down the digestion and absorption of glucose. You may notice that your blood glucose peaks between 1 and 2 hours after eating, which is a normal response.
However, if you eat a sugary snack or treat on its own, your glucose levels will likely peak around 30 minutes after eating. With decreased insulin sensitivity, you may see that your glucose doesn’t peak until one or even two hours after eating the sweet snack.6
The Time Your Glucose Spends Above Average
Your glucose should return to a baseline that’s typically between 70 and 100 mg/dL within 2-3 hours of eating. A 2025 study found that metabolically healthy people typically spend 95 percent of their time in range (TIR) between 70 and 140 mg/dL, indicating strong metabolic health.6
Frequency of Glucose Spikes
Eating foods or meals that lead to frequent blood sugar spikes without allowing your blood sugar to return to baseline can keep your glucose and insulin levels consistently elevated. If your CGM shows you're never quite returning to baseline before your next meal, you're maintaining chronically elevated insulin levels that could be blocking fat loss.
Understanding Your CGM Patterns and Adjusting Your Diet To Reach Your Goals
Once you’ve gathered data on how your glucose responds to the foods you eat, it’s time to start experimenting. Rather than eliminating entire food groups, a CGM lets you strategically experiment and learn what actually works to support your metabolism.
Test Portion Sizes
Instead of cutting out a food completely, test different portion sizes. You might find that ⅓ cup of rice with dinner keeps you in range, while 1 cup results in a larger or longer spike. Try combining different portions of carbohydrate foods with your meals to figure out what makes the most sense to leave you satisfied and full, and to keep your glucose and insulin levels stable.
Experiment with Food Order
Recent research shows that eating protein and vegetables before carbohydrates in the same meal can reduce glucose spikes by almost 30% compared to eating carbs first, and improve time in range.7,8 If you notice consistent spikes from meals containing rice, pasta, bread, or even fruit, try adjusting the food order by eating your protein and vegetables first, then enjoy the carbohydrate at the end of the meal.
Experiment with Activity
Exercise has immediate and long-term effects on blood glucose and insulin sensitivity. Research shows that while exercise will immediately help reduce glucose levels, as your muscles have improved uptake of glucose from the bloodstream, you may notice an increase in insulin sensitivity for up to 72 hours after exercise.9
Also, keep in mind that regular exercise can improve insulin sensitivity overall. One small study found that eight weeks of regular aerobic and strength exercise significantly improved insulin sensitivity in healthy young women.10
Get Strategic with Food Swaps
Rather than generic "healthy" substitutions, use your CGM data to find swaps that actually work for your body. If whole wheat bread spikes your glucose similarly to white bread, that swap isn't helping you. Test alternatives systematically: sourdough, sprouted grain, or switching up the foods you pair with it. You can use this data to find lower-impact foods you actually enjoy and want to eat long-term.
Stay Focused on Patterns and Context
As you’re analyzing data and experimenting, keep in mind that the same food or meal can produce different glucose responses depending on a lot of other factors. A banana eaten alone might spike your glucose significantly, while the same banana eaten after a meal with protein and fat may produce a much gentler curve.
Your stress levels, sleep quality the night before, where you are in your menstrual cycle (for women), and your activities that day can all influence how your glucose responds. A CGM reveals these patterns so you can adjust accordingly rather than following rigid rules.
Topics discussed in this article:
References
- https://www.mdpi.com/1422-0067/25/10/5488
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7337187/
- https://www.nature.com/articles/s41598-025-08003-4#
- https://www.e-dmj.org/journal/view.php?number=2614
- https://www.mayoclinic.org/diseases-conditions/obesity/multimedia/vid-20536756
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6215929/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4876745/
- https://diabetesjournals.org/care/article/48/2/e15/157633/Carbohydrates-Last-Food-Order-Improves-Time-in
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8352615/
- https://www.nature.com/articles/s41598-025-86306-2


.jpg)

.svg)





.webp)

.jpg)

.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
