Key Takeaways
- Sleep needs change with age, but quality sleep is essential at all stages of life.
- Consistent sleep supports glucose regulation and metabolic health.
- Simple habits like regular bedtimes and balanced meals, all tracked through the Signos app, can help improve sleep and metabolic resilience.
that {{mid-cta}}
Sleep needs change right along with you, from the long, restorative stretches required in childhood to the shorter, sometimes fragmented sleep more common in adulthood and beyond.1,2,3
Understanding how sleep requirements vary by age can help you support your own health, energy, and metabolic stability, and better care for the people you love.
In this article, we explore how sleep changes from infancy through older adulthood, what drives those shifts, and how sleep quality impacts overall health at every stage.
Why Sleep Needs Change With Age

From birth until late adolescence, the human brain and body develop rapidly and strive towards maturation. During this time, long, consolidated sleep is needed to support this rapid growth, and the body is more efficient at encouraging quality sleep.1,2,3
As we age, our sleep architecture changes, meaning we get less deep sleep (slow-wave and REM), more fragmented sleep, more frequent awakenings, and more daytime napping.2,3
Our circadian rhythm (the body’s internal 24-hour clock) changes in response to hormonal shifts, such as decreased growth hormone and melatonin, and altered cortisol levels, all of which make it harder to fall asleep and stay asleep.2,3
On top of that, lifestyle factors that accumulate over time further complicate sleep. Adults shoulder a load that includes parental responsibilities, job stress, atypical work hours, caregiving for aging relatives, and financial insecurity, all of which can worsen sleep quality.2,3
Normal adult aging includes shorter total sleep time, lighter sleep, and increased awakenings, but the body still requires a set amount of high-quality sleep for overall health and well-being. Understanding these changes and the importance of healthy sleep across all ages can help guide you to make adjustments to your sleep habits, environment, and lifestyle.1,2,3

How Sleep Quality Changes With Age
Sleep and achieving quality sleep often begin to feel different and more elusive as we get older. In childhood and adolescence, the body was primed for deep, restorative sleep to support rapid growth and brain development, often reinforced by predictable routines and caregiver-guided sleep hygiene.1-4
As we age, however, both internal changes and external lifestyle factors can interfere with the ability to achieve consistent, quality sleep.
A large body of research across many populations shows that aging is associated with:
- A reduced proportion of slow-wave (deep) and REM sleep2
- More frequent and prolonged nighttime awakenings (time to fall back asleep)2,3
- Lower sleep efficiency (actual time spent asleep in bed)2,3
- A shift towards earlier bedtimes and wake-up times in older adults2,3
- Increased sensitivity to environmental disruptions (noise, light, or room temperature)2,3
- A higher risk of sleep disorders, insomnia, or sleep fragmentation2,3
These internal and external factors make it more challenging to achieve restorative sleep. Over time, chronic poor sleep can negatively affect our metabolic health, increase the risk of chronic conditions like heart disease, diabetes, obesity, and mental health issues, and impair cognitive and immune function.5
How Sleep Impacts Metabolic and Glucose Health

Sleep and metabolic health, including glucose health, are intricately connected.
A 2021 article reviews evidence linking sleep duration to increased obesity and risk of type 2 diabetes, finding that short sleep (particularly chronic poor sleep of less than six hours) is associated with a 55% higher risk of becoming obese and a 28% increased risk of developing type 2 diabetes.6
Additionally, after just 4 to 5 nights of short sleep (or sleep deprivation), glucose levels increased, and insulin sensitivity decreased by 20 to 30%, highlighting the detrimental effects of poor sleep on glucose health!6
When you don’t get enough sleep regularly, several hormones that control hunger, appetite, and metabolism are affected. Ghrelin (a hunger hormone) increases, and leptin (a satiety hormone) decreases, making you feel hungrier after poor sleep. Studies show that ghrelin is 14% higher in short sleepers compared to normal sleepers.6
Furthermore, chronic sleep loss can shift cortisol levels and rhythms, disrupting blood glucose levels. Adequate sleep helps to regulate cortisol levels and protect against metabolic disruptions.6
In a study of 1,156 adults using a CGM to monitor sleep and glucose levels, persistent inadequate sleep and late bedtimes were associated with greater glucose variability compared to adequate sleepers.7
Emerging research indicates that consistent sleep in chronically sleep-deprived individuals improves glucose metabolism (improved insulin resistance and beta-cell function) after 2 weeks of sleeping for more than 6 hours.8
Maintaining consistent, adequate sleep improves metabolic resilience across all ages and helps prevent chronic disease.5-8
Signos Insights: Tracking Sleep’s Impact on Your Metabolism
.png)
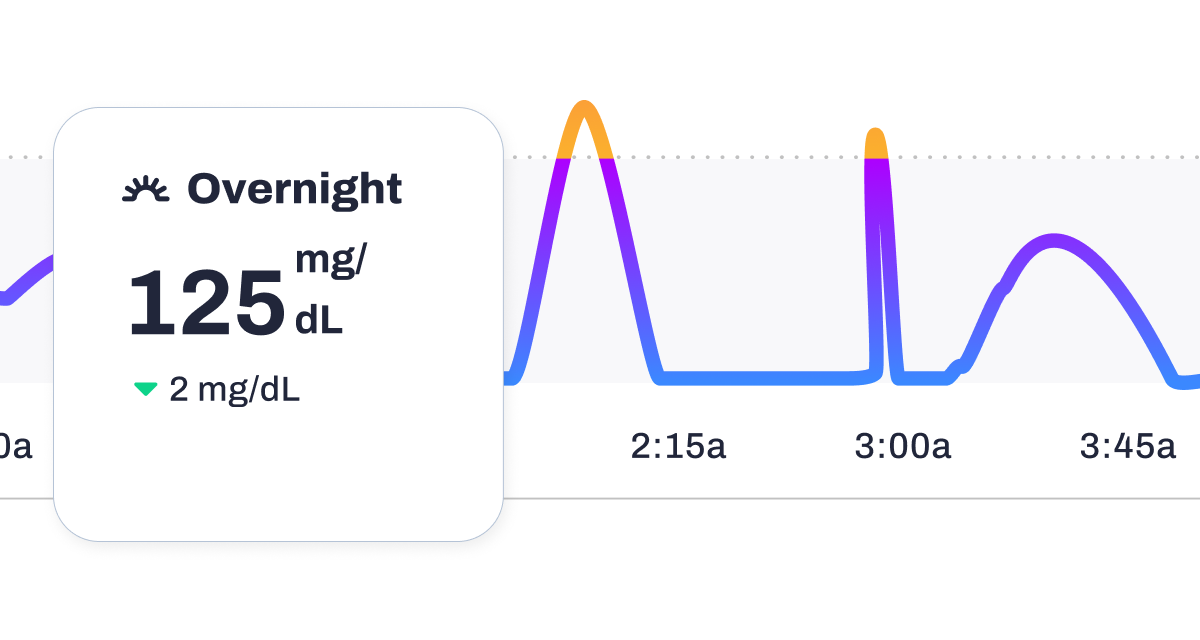
Sleep isn’t just recovery; it’s a metabolic regulator. With a CGM and the Signos app, you can see how sleep duration, timing, and consistency shape your glucose patterns the next day and beyond.
Key Signals to Monitor in Signos
Overnight glucose trends
Your CGM captures what happens while you sleep, when food and movement are removed from the equation. Look for:
- Stable overnight plateaus (purple zone), often linked to adequate sleep and lower stress.
- Gradual upward drift or early-morning rises can signal short sleep, late meals, alcohol, or elevated cortisol.
- Greater morning variability may predict higher glucose responses to breakfast.
Weekly Insights
Signos’ Weekly Insights help connect sleep patterns to downstream effects:
- Higher glucose variability (GV) following inconsistent bedtimes or short sleep.
- Increased morning glucose spikes on poor-sleep days.
- Correlations between disrupted sleep and reported cravings, lower energy, or reduced movement.
By zooming out to the week, you can see whether sleep habits are quietly shaping your metabolism, even when meals stay the same.
Sleep Experiments to Try in Signos
Use Signos’ experiment mindset to isolate what actually helps your metabolism.
1. Sleep Duration Experiment: 6 vs. 8 Hours
- Hold meals and activities as steady as possible.
- Compare overnight glucose stability and next-morning responses.
- Watch for differences in breakfast spikes and overall daily GV.
2. Bedtime Timing Experiment: Earlier vs. Later
- Test an earlier bedtime for 3–5 nights, then a later one.
- Note changes in overnight glucose drift and morning baseline.
- Many members see steadier overnight curves with earlier sleep timing.
3. Caffeine Cut-Off Experiment
- Try stopping caffeine by noon vs. mid-afternoon.
- Log both sleep quality and next-day glucose.
- Look for reduced overnight variability or smoother morning transitions.
4. Evening Routine Experiment
Test one variable at a time:
- Magnesium supplementation
- Evening protein instead of carbs
- Reduced screen time in the last hour
Track how each impacts overnight glucose smoothness and morning stability.
Context Logging: Turn Patterns Into Proof
Tag sleep quality, bedtime, wake time, and evening behaviors directly in the Signos app. Over time, these context logs:
- Reveal repeatable patterns across weeks.
- Help explain “why” certain days feel harder metabolically.
- Turn subjective sleep quality into measurable metabolic insight.
With individualized sleep insights (not generic advice), Signos helps you build metabolic resilience that fits your real life, not an ideal schedule.
The Bottom Line
Your sleep needs shift throughout your life, and sleep quality naturally shifts with age, but prioritizing consistent, quality rest is essential at every stage of life.
Adequate sleep supports metabolic and glucose health. Understanding your sleep needs and patterns, alongside implementing practical habits like consistent bedtimes and avoiding external factors that reduce sleep, will help support steadier energy, better recovery, and long-term well-being.
Learn More With Signos’ Expert Advice
A CGM can help you link your sleep patterns and glucose levels and nudge you towards better sleep and metabolic resilience to improve your overall health. Learn more about glucose levels and tracking on the Signos blog, written by health and nutrition experts.
Topics discussed in this article:
References
- https://pubmed.ncbi.nlm.nih.gov/27707447/
- https://pubmed.ncbi.nlm.nih.gov/29412976/
- https://pubmed.ncbi.nlm.nih.gov/40538866/
- https://pubmed.ncbi.nlm.nih.gov/29073398/
- https://www.ncbi.nlm.nih.gov/books/NBK19961/
- https://pubmed.ncbi.nlm.nih.gov/34779405/
- https://pubmed.ncbi.nlm.nih.gov/40042843/
- https://pubmed.ncbi.nlm.nih.gov/31053213/




.svg)







.jpg)
.jpg)
.webp)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
