GLP-1 medications are among the most widely used agents for improving glycemic control and supporting metabolic health. In the United States alone, more than 1 in 8 adults has used a GLP-1 medication such as semaglutide or tirzepatide in recent years.1 As more people start these medications, we also see that more people are reaching the point where tapering or discontinuation becomes part of their care plan.
For many people, reducing or stopping GLP-1 therapy can lead to noticeable changes in appetite, energy, and glucose levels.2 Some see higher fasting glucose, larger post-meal spikes, or more day-to-day variability than they experienced while on medication. These shifts can feel confusing, especially if your lifestyle habits have not otherwise changed.
Let’s dive into how tapering off a GLP-1 medication can affect your blood sugar, and what you can focus on if stabilizing your glucose levels is your goal.
How GLP-1 Medications Affect Blood Sugar
.jpg)
GLP-1 medications work by supporting several key systems that help stabilize blood sugar. They affect insulin release, digestion, appetite signals, and the body's handling of blood sugar after meals.3 Together, these effects often lead to smoother glucose patterns and fewer spikes throughout the day.
Here’s how they impact blood sugar regulation:
- Glucose variability: GLP-1 medications help reduce large swings in blood sugar levels. They slow digestion and improve the timing of insulin release, leading to steadier post-meal glucose curves rather than sharp highs and crashes.
- Insulin sensitivity: They also improve insulin's effectiveness, especially after eating. When cells respond better to insulin, glucose is removed from the bloodstream more efficiently. This reduces the amount of insulin needed to control blood sugar and lowers your total glucose levels.
- Appetite control and blood sugar management: GLP-1 medications dim your hunger signals and increase feelings of fullness. As a result, eating smaller, more balanced meals often leads to fewer rapid glucose rises. Though this plays a role indirectly by affecting your food intake, many notice that their daily glucose patterns improve as a result.
Reasons for Tapering Your GLP-1
.jpg)
People choose to taper GLP-1 medications for many different reasons. There isn’t a single “right” timeline. The decision usually depends on health goals, side effects, accessibility, and long-term sustainability.4 What matters most is having a clear plan so glucose stability and metabolic health don’t take a sudden hit.
Common reasons for tapering include:
- You reached your health or weight goal: Some individuals taper off GLP-1 after achieving a target weight or metabolic improvement and transition to a maintenance phase supported solely by lifestyle habits. Notably,
- Side effects or tolerance issues: Nausea, gastrointestinal discomfort, fatigue, or other side effects may become difficult to manage over time, leading people to reduce or discontinue use.
- Medication preferences: Some individuals prefer to limit long-term medication use or want to avoid ongoing injectable therapy.
- Cost or insurance coverage changes: Access and affordability remain major factors in long-term GLP-1 use. Changes in insurance coverage or high out-of-pocket costs often affect whether you can afford to continue your GLP-1 medication and dose.
- Life-stage changes: Certain life stages are not amenable to GLP-1 therapy. Pregnancy planning, breastfeeding, medical procedures, or new medical diagnoses may require pausing or adjusting your GLP-1 plan.
- Plateauing or diminishing response: Some individuals experience less noticeable benefits over time and mayreassess their treatment plan.
What Happens After Getting Off a GLP-1 Medication
.jpg)
When you taper off a GLP-1 medication, your body has to adjust to running without the extra hormonal support that helped regulate appetite and blood sugar while taking the medicine. Think of it like taking training wheels off a bike. You can still ride, but your body’s balance and feelings of control may feel different at first.
The most common changes people notice include:2
- Increased appetite and hunger signals: GLP-1 medications reduce hunger hormones and slow digestion. As doses decrease, these effects fade, and hunger cues may return closer to baseline.
- Greater glucose variability: Without medication support, postprandial blood glucose spikes and fasting glucose changes may become more pronounced, particularly if insulin sensitivity is reduced.
- Energy fluctuations: Some people experience energy challenges as blood sugar patterns shift.
- Food cravings and food noise: Food noise, or the constant chatter in the mind about what to eat, how much, and when, can recur during withdrawal from GLP-1 medication. For some, this is a huge hurdle in maintaining weight loss post-GLP-1 therapy.
- Changes in fullness and portion tolerance: Your meals may feel less filling than before, which can lead to changes in portion sizes and eating habits.
This is why tapering slowly is important. Reducing your dose gradually allows your body time to adapt. It helps prevent sharp appetite rebounds, extreme hunger, and sudden glucose instability. Going “cold turkey” often leads to larger swings in blood sugar and significant rebound weight effects.
If your plan is to taper off your GLP-1 medication, it is important to work closely with your prescribing medical provider. They can help create a step-down schedule, monitor symptoms, and adjust your plan if glucose levels or side effects change.
What Increases Glucose Variability Post-GLP-1?
While GLP-1 therapy improves insulin signaling and slows glucose release into the bloodstream, those benefits fade as the dose is reduced. Once this support is removed, your body may struggle to manage blood glucose after meals, leading to higher fasting blood glucose in the morning or sharper postprandial spikes.
Everyone’s body responds differently after tapering a GLP-1 medication. If you have pre-existing type 2 diabetes or prediabetes, you may have some degree of insulin resistance, and thus, when weaning off the medication, your body may not respond to insulin as efficiently.2
Lifestyle Factors That Affect Glucose After GLP-1
.jpg)
After tapering a GLP-1 medication, your daily habits play an even bigger role in keeping blood sugar stable and maintaining your progress. Without medication doing some of the work behind the scenes, your lifestyle becomes the main “control panel” for glucose regulation. Small choices around food, sleep, stress, and movement can add up to meaningful differences in glucose patterns.
If weaning off your GLP-1 medication is your goal, spending some time building solid lifestyle habits first can help prevent glucose instability and weight regain later.
These key lifestyle factors influence your blood sugar post-GLP-1 use:
- Meal composition: Balanced meals that include protein, fiber, and healthy fats help slow digestion and reduce rapid glucose rises. Meals high in refined carbohydrates and low in protein or fiber tend to cause larger post-meal glucose spikes.
- Meal timing and consistency: Skipping meals or eating erratically can increase glucose variability. Consistent meal timing helps regulate hunger hormones and supports more stable blood glucose levels throughout the day.
- Physical activity: Movement improves insulin sensitivity by helping muscles use glucose more efficiently. Even light activity, such as walking after meals, can reduce post-meal glucose spikes.
- Sleep quality: Poor sleep increases insulin resistance and stress hormones like cortisol, which can raise fasting and morning glucose levels.
- Stress levels: Chronic stress triggers the cascade of hormones that raise blood sugar by signaling the liver to release stored glucose. Managing your stress response helps stabilize your glucose levels.
- Hydration: Mild dehydration can raise blood glucose levels and impair circulation.
Using CGM After GLP-1 to Track Blood Sugar Patterns
.png)
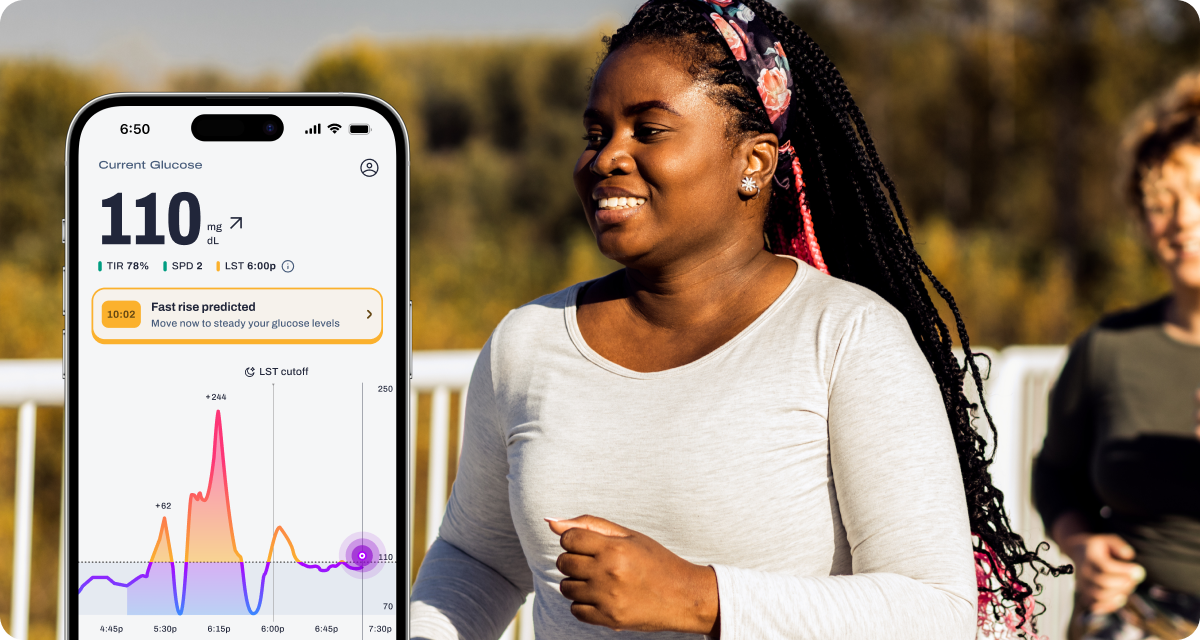
After tapering a GLP-1 medication, it can be challenging to understand what’s driving changes in hunger, energy, or cravings. Appetite signals may feel less predictable, and without clear feedback, it’s easy to mistake normal adjustment for setback. This is where continuous glucose monitoring (and Signos) can provide clarity.
CGMs allow you to see real-time blood sugar patterns tied to everyday behaviors, including meals, sleep, stress, and physical activity. With Signos, members can observe how their body responds as appetite suppression decreases and metabolic signals rebalance. For example, CGM data can reveal which meals elicit larger postprandial glucose spikes, whether fasting glucose rises after poor sleep, or how quickly glucose recovers when light physical activity is added after meals.
Signos helps turn this data into insight through personalized Weekly Insights and experiments, designed to support stability during and after GLP-1 tapering:
- Meal composition experiments help members compare glucose responses to meals higher in protein and fiber versus refined carbohydrates, supporting satiety as medication effects change.
- Postprandial movement experiments test the impact of short walks or light activity after eating, often improving glucose recovery and reducing energy dips.
- Sleep and recovery experiments identify how inconsistent sleep or elevated stress influences morning glucose and next-day hunger.
- Glucose variability tracking highlights increased swings between highs and lows, a common pattern after GLP-1 tapering that can contribute to cravings and fatigue.
By making glucose variability visible, Signos helps members identify early signals that adjustments are needed, before frustration or weight regain sets in. Instead of relying on willpower alone, members can use real-time feedback and habit tracking to reinforce behaviors that support steadier glucose, more consistent energy, and sustainable routines beyond medication.
FAQs
- What happens to blood sugar after tapering GLP-1? Blood sugar may rise or become more variable as the effects of appetite suppression and insulin sensitivity decrease, especially around meals and during fasting periods.2
- Can CGM help after stopping GLP-1? Yes, CGMs help identify patterns in glucose responses related to food, sleep, stress, and activity, making it easier to adjust your personal habits.
- Why do glucose spikes happen after GLP-1 use? GLP-1 medications slow down digestion and improve insulin response, so when these effects fade, post-meal glucose can rise quickly. This is especially true if eating patterns and lifestyle habits are not adjusted during weaning from a GLP-1.2
- How long does glucose instability last after GLP-1? This varies depending on your personal health history, but many people notice changes over several weeks as the body adapts to lower medication doses and establishes a new metabolic baseline.
- How can glucose be stabilized after tapering GLP-1? Glucose stability can improve with consistent meals, adequate protein and fiber intake, regular physical activity, good sleep, and stress management.
Read Next: How to Safely Transition Off a GLP-1
Topics discussed in this article:
References
- Harris E. Poll: Roughly 12% of US Adults Have Used a GLP-1 Drug, Even If Unaffordable. JAMA.2024;332(1):8. doi:10.1001/jama.2024.10333
- Tzang CC, Wu PH, Luo CA, et al. Metabolic rebound after GLP-1 receptor agonist discontinuation: a systematic review and meta-analysis. EClinicalMedicine. 2025;90:103680. Published 2025 Nov 28. doi:10.1016/j.eclinm.2025.103680
- Collins L, Costello RA. Glucagon-Like Peptide-1 Receptor Agonists. [Updated 2024 Feb 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551568/
- Mozaffarian D, Agarwal M, Aggarwal M, et al. Nutritional Priorities to Support GLP-1 Therapy for Obesity: A Joint Advisory From the American College of Lifestyle Medicine, the American Society for Nutrition, the Obesity Medicine Association, and the Obesity Society. Am J Lifestyle Med. Published online May 30, 2025. doi:10.1177/15598276251344827


.webp)
.svg)










.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
