Key Takeaways
- Stopping GLP-1 medications can lead to changes in appetite, cravings, blood sugar, and energy levels, especially if discontinued abruptly.
- Gradual tapering is often recommended to help ease appetite spikes and gastrointestinal side effects.
- Strong nutrition habits, such as prioritizing protein, fiber, and consistent meals, are essential as medication effects wear off.
- Physical activity, especially strength training and consistent activity, helps preserve lean muscle and supports metabolic flexibility after discontinuation.
- Monitoring glucose, energy, and appetite patterns can provide helpful insight as your body establishes a new baseline.
- Ongoing support from healthcare providers and tools like Signos can make the transition feel more manageable and grounded in data rather than guesswork.
that {{mid-cta}}
Stopping a GLP-1 medication can feel unsettling, especially if it helped you quiet food noise, regulate your appetite, and support weight loss. Many people worry about weight regain, more food cravings, or losing the structure that the medication once provided.
GLP-1 drugs like Ozempic, Wegovy, and Zepbound work by changing how the body regulates hunger and blood sugar, so it makes sense that stopping them brings noticeable shifts. At the same time, stopping these medications is sometimes necessary due to side effects, cost, or simply personal preference. The good news is that with thoughtful planning, nutrition support, and attention to lifestyle habits, you can transition off GLP-1 medications in a way that supports metabolic health and helps you find a new, stable baseline.
Why Weight or Appetite May Change After Stopping GLP-1

GLP-1 medications work by changing how your body regulates hunger, fullness, and blood sugar. While you’re taking GLP-1 drugs, your appetite is typically lower, food noise is quieter, and you may feel full faster because gastric emptying slows down. These effects are drug-induced, meaning they fade once the medication is reduced or stopped.
After discontinuing the medication, it’s common for appetite to gradually return toward your natural baseline. This reflects how glucagon-like peptide-1 receptor agonists interact with the brain and gut while they’re active. Some people notice stronger hunger cues or increased cravings during this transition, especially if they stop cold turkey rather than tapering under healthcare guidance.
Importantly, weight regain can happen if lifestyle changes haven’t been fully established while on the medication. GLP-1 treatment supports weight loss and weight management, but it doesn’t permanently alter the body’s metabolism on its own. Without healthy lifestyle habits that support satiety, blood sugar balance, and lean muscle mass, body weight may trend upward over time.
For people using GLP-1 medications, particularly for type 2 diabetes or obesity, blood sugar or blood pressure may also trend differently after stopping. That’s why following up with a healthcare provider and a dietitian is an important part of stopping GLP-1s safely and protecting your long-term health.
6 Steps to Safely Stop a GLP-1

1. Consult Your Provider
Stopping or tapering GLP-1 medications should always be done under your prescribing healthcare provider's guidance. These medications affect appetite, digestion, blood sugar, and hormones that regulate hunger, so stopping suddenly, especially going “cold turkey”, can feel hugely disruptive. A provider can help you anticipate changes in appetite, energy, and glucose control, and develop a plan to protect your health.
This is also the time to discuss whether other supportive tools will be helpful, such as nutrition counseling, alternative medications, or closer follow-up. For people using GLP-1s for type 2 diabetes, obesity, or cardiometabolic risk, coordination with your healthcare team is especially important to avoid unwanted blood sugar or blood pressure changes during your transition.
2. Gradual Taper
Many providers recommend tapering the dose rather than stopping abruptly. This is especially true if you have diabetes or blood sugar concerns. Reducing the dose gradually may help buffer against big appetite increases, reduce gastrointestinal side effects, and give your body time to recalibrate hunger and satiety signals as GLP-1 effects fade.
While not everyone needs a taper, research and clinical experience suggest that easing off slowly can reduce sudden spikes in cravings or food noise. If tapering is part of your plan, pair it with close self-monitoring so adjustments can be made based on how your body responds, as weight regain is the most common side effect of discontinuing these medications.1
3. Strengthen Nutrition Habits
As your appetite returns, your nutrition habits become the main driver of weight management. Building your meals around protein, fiber, and healthy fats helps support satiety and steady blood sugar after stopping GLP-1 treatment. Plus, aim for regular meals rather than skipping or grazing, as this can increase cravings and lead to overeating later in the day.2 You’ll also want to limit ultra-processed foods and sugary drinks to help reduce rapid glucose swings that may drive hunger.
4. Prioritize Physical Activity
Physical activity plays a key role in protecting against weight regain after stopping GLP-1 drugs. You might even consider working on this habit before you stop the medication. Having a strong foundation of regular activity can help prevent weight regain.
Strength training is especially important because it helps preserve lean muscle mass, which supports metabolic flexibility and resting energy expenditure.3 Walking and general activity throughout the day matter too. Staying active, even in little ways, plays a major role in boosting metabolism. This phenomenon is also referred to as non-exercise activity thermogenesis.4
5. Track Energy and Glucose
Tracking your energy and blood sugar levels can provide valuable feedback as your body adjusts to not having GLP-1 medications. Consider using tools like a continuous glucose monitor (CGM) with Signos to help you notice patterns in blood sugar, energy, and appetite that may shift after medication changes.5
6. Behavioral and Mindset Shifts
Coming off GLP-1s isn’t just a physical change, but likely also an emotional one. Mindful eating strategies, such as slowing down at meals and checking in with hunger and fullness cues, can help you respond to appetite changes without fear or judgment.6
Stress management also matters here, especially if you have a history of emotional eating. Research shows that chronic stress increases emotional eating and weight gain.7 Plus, setting realistic expectations, like aiming for weight maintenance rather than continued loss, can reduce pressure and support a healthier relationship with food as your body finds its new equilibrium.
How to Minimize Weight Regain Post-GLP-1

To recap, here are the “big rocks” to focus on while tapering off your GLP-1 medication to prevent weight re-gain:
- Maintain consistent meal structure: Eating regular meals (rather than skipping or grazing) helps regulate appetite hormones, stabilize blood sugar, and reduce sudden hunger or cravings as medication effects wear off.
- Prioritize protein and fiber: Including them at each meal supports satiety, helps manage food noise, and slows digestion. These building blocks of your meals become even more important as appetite returns toward baseline.
- Track weight and glucose trends: Checking weight weekly and observing glucose patterns with tools like Signos can help you notice changes early and adjust habits before small shifts turn into larger challenges.
- Plan exercise around energy and appetite cues: Aligning physical activity with times you feel most energized can make movement more sustainable and help offset changes in appetite or energy expenditure.
- Lean on professional support: Ongoing guidance from a dietitian, functional provider, or health coach can help personalize nutrition, activity, and mindset strategies during discontinuation and beyond.
How Signos Can Help During Transition
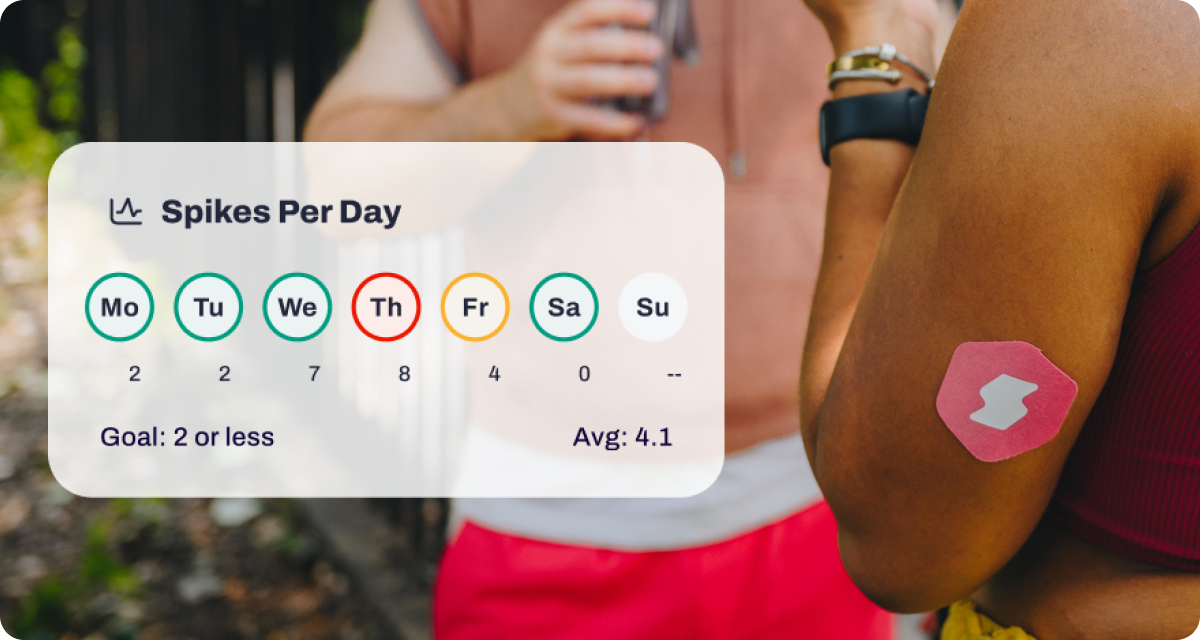
Stopping a GLP-1 medication can shift appetite, energy, and glucose control. Signos provides objective, real-time feedback so you can respond early, before small changes turn into setbacks.
- 24/7 Glucose Monitoring: As medication effects fade, continuous glucose data shows how your body responds to meals, snacks, and timing changes. This helps you adjust portion sizes, meal composition, and eating windows based on what actually keeps your glucose steadier.
- Weekly Insights: Signos’ Weekly Insights reports surface patterns in glucose variability, energy dips, and post-meal responses over time. Seeing trends, not just single spikes, makes it easier to course-correct food and activity habits as appetite cues change.
- Guided Experiments: Use structured experiments to test strategies that support satiety and stability during the transition, such as:
- Eating protein or fiber first to blunt post-meal spikes
- Shifting carbohydrate intake earlier in the day
- Adding a 5–10 minute walk after meals
- Comparing three meals vs. smaller, more frequent meals
Glucose feedback shows which habits help maintain steadier energy and reduce rebound hunger. Together, these features turn uncertainty into clarity, helping you build sustainable habits as your body recalibrates without GLP-1 support.
The Bottom Line
Transitioning off a GLP-1 medication works best when it’s done with intention, support, and realistic expectations. Focusing on nutrition quality, consistent movement, and behavior skills, while monitoring how your body responds, can help protect metabolic health during this transition. Working closely with your healthcare team and using supportive tools can make stopping GLP-1s feel manageable rather than overwhelming.
Learn More With Signos’ Expert Advice
Signos offers science-backed tools to support overall wellness by helping you understand how daily habits affect glucose and energy levels. Learn more about how Signos can support health and explore educational resources on glucose patterns and metabolic insights on the Signos blog to stay informed and feel empowered during your transition.
Topics discussed in this article:
References
- Berg S, Stickle H, Rose SJ, Nemec EC. Discontinuing glucagon-like peptide-1 receptor agonists and body habitus: A systematic review and meta-analysis. Obes Rev. 2025 Aug;26(8):e13929. doi: 10.1111/obr.13929.
- Lopez-Minguez J, Gómez-Abellán P, Garaulet M. Timing of Breakfast, Lunch, and Dinner. Effects on Obesity and Metabolic Risk. Nutrients. 2019;11(11):2624. Published 2019 Nov 1. doi:10.3390/nu11112624
- Westcott WL. Resistance training is medicine: effects of strength training on health. Curr Sports Med Rep. 2012 Jul-Aug;11(4):209-16. doi: 10.1249/JSR.0b013e31825dabb8.
- von Loeffelholz C, Birkenfeld AL. Non-Exercise Activity Thermogenesis in Human Energy Homeostasis. [Updated 2022 Nov 25]. In: Feingold KR, Adler RA, Ahmed SF, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000.
- Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc. 2011;111(1):92-102. doi:10.1016/j.jada.2010.10.008
- Nelson JB. Mindful Eating: The Art of Presence While You Eat. Diabetes Spectr. 2017;30(3):171-174. doi:10.2337/ds17-0015
- Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. 2007 Nov-Dec;23(11-12):887-94. doi: 10.1016/j.nut.2007.08.008.



.webp)
.svg)


.jpg)







.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
