Key Takeaways
- Type 1 diabetes is an autoimmune disease in which the body attacks insulin-producing beta cells in the pancreas, requiring lifelong insulin therapy.
- Type 2 diabetes develops over time due to insulin resistance and can often be delayed or managed through lifestyle changes, medication, or both.
- Prediabetes is an early warning sign with elevated blood sugar levels, not yet diabetes, but a critical opportunity to take action.
- Recognizing early symptoms, getting regular lab tests, and understanding risk factors (such as family history or lifestyle) are key to early detection.
- Tools like continuous glucose monitors (CGMs) and personalized insights can support better decision-making and blood sugar control at every stage.
that {{mid-cta}}
Diabetes is one of the most common chronic health conditions in the U.S., but many people are surprised to learn there’s more than one kind. In fact, the types of diabetes, type 1, type 2, and prediabetes, each have different causes, risk factors, and treatment strategies.
Whether you’re navigating a recent diagnosis, supporting a loved one, or simply trying to stay informed, understanding the differences can make a big impact on your health. We’ll break down what sets each type apart, how to spot early signs of blood sugar dysregulation, and practical steps you can take to support a healthy metabolism no matter where you are in your journey.
What Is Type 1 Diabetes?
-min.jpg)
Type 1 diabetes is an autoimmune disease that often begins in childhood or young adulthood, although it can happen at any age. In people with type 1 diabetes, the immune system mistakenly attacks the insulin-producing beta cells in the pancreas. Without enough insulin, glucose (sugar) builds up in the bloodstream because it can’t enter the body’s cells to be used for energy.1
People with type 1 diabetes often notice symptoms develop quickly, sometimes over just a few weeks. Common signs include increased thirst, frequent urination, unexplained weight loss, extreme hunger, blurry vision, and fatigue. Some people also experience nausea or stomach pain. Because the body can’t make enough insulin, glucose builds up in the bloodstream, and these early symptoms are the body’s way of signaling that something isn’t right.
Unlike type 2 diabetes, which is often tied to lifestyle and develops over time, type 1 diabetes requires daily insulin for life after diagnosis. While lifestyle habits still play a meaningful role in managing blood sugar levels and overall health, people with type 1 will always need to use insulin.
Technology has made it easier than ever to manage blood glucose levels with tools like continuous glucose monitors (CGMs) and insulin pumps. These devices provide more consistent data and reduce the guesswork in daily diabetes care for folks with type 1.
What Is Type 2 Diabetes?

Type 2 diabetes is the most common form of diabetes and typically develops later in life, though more young adults and even teens are being diagnosed today. It happens when the body becomes resistant to insulin over time, making it harder for glucose to move out of the bloodstream and into the body’s cells. Eventually, the pancreas may not be able to make enough insulin to keep blood sugar levels in a healthy range.2
Unlike type 1 diabetes, symptoms of type 2 diabetes often appear gradually. You may feel more tired than usual, experience increased hunger or thirst, notice slower wound healing, or have blurry vision. Many people don’t realize they have it until a routine blood test reveals high blood sugar levels or an elevated A1C.
The good news is that type 2 diabetes can often be managed, and even delayed or prevented with lifestyle changes, especially when detected early. Nutrition, regular physical activity, stress management, and quality sleep all play a role. In some cases, oral medications or insulin therapy may also be needed.
Here are some ways to manage type 2 diabetes and improve blood sugar levels:
- Build your meals around protein, healthy fats, fiber, and complex carbohydrates.
- Move your body daily. Aim for a mix of cardio and strength training.
- Prioritize sleep and manage stress, both of which impact glucose when we aren’t taking care of ourselves.
- Check your blood sugar at least once a day, or consider using a continuous glucose monitor to see real-time data throughout the day.
- Take your medications as prescribed and stay in touch with your healthcare provider about any changing symptoms.
- Get regular labs to monitor your A1C and blood glucose levels.
What Is Prediabetes?

Prediabetes is the early stage of blood sugar dysregulation when glucose levels are higher than normal but not high enough to meet the criteria for type 2 diabetes. It’s a warning sign from your body that something’s off with how you process insulin and manage blood sugar. If you’re in the pre-diabetic range, the pancreas may still produce insulin, but the body isn’t using it as effectively as it should.3
The tricky part is that most people with prediabetes don’t notice any major symptoms. In fact, it’s estimated that almost 90% of people with prediabetes don’t know they have it.4 You might feel more tired, hungrier than usual, or crave carbs more often, but it’s easy to miss or chalk it up to a busy week. That’s why early detection through lab work, like elevated fasting glucose or A1C, is so important.
The good news is that this is a highly reversible stage. With small, consistent changes to your daily habits, you can improve your blood sugar levels and lower your risk of developing type 2 diabetes.
Here are some strategies that help manage and reverse prediabetes:
- Focus meals around lean protein, fiber-rich foods, and healthy fats.
- Incorporate physical activity you enjoy. Even simple activities like walking count.
- Get at least 7 to 9 hours of quality sleep.
- Reduce stress through hobbies, breathwork, or movement.
- Ask your healthcare provider to monitor your labs regularly, and consider using a continuous glucose monitor for real-time feedback.
Key Differences: Type 1 vs Type 2 vs Prediabetes
Remember that while all three types of diabetes affect how your body manages glucose, the root causes and treatments are very different. Understanding these differences can help you take the right steps for prevention, early detection, or better management.
Here’s a quick breakdown

Early Detection and Prevention Strategies

Catching blood sugar changes early can make a big difference, especially with type 2 diabetes and prediabetes, where lifestyle changes can delay or even prevent progression.
The best first step: always keep your annual physical. A simple blood test every year can screen your A1C, glucose levels, and other key markers to flag early signs of blood sugar dysregulation.
Here are a few ways to stay ahead:
- Know your numbers. Ask your healthcare provider to check your A1C and fasting blood glucose levels at your next appointment.
- Move your body regularly. Physical activity helps your body use insulin more effectively. Aim for a walk after meals or any movement you enjoy.
- Build balanced meals. Focus on fiber-rich carbs (such as whole grains and veggies), lean protein, and healthy fats to help stabilize blood sugar.
- Prioritize sleep and manage stress. Lack of sleep and high stress can raise blood sugar levels, even if your diet is on point.
- Pay attention to early signs. Feeling extra tired, thirsty, or noticing more cravings lately? These could be subtle signs your blood sugar is shifting.
How Signos Supports People Across the Spectrum
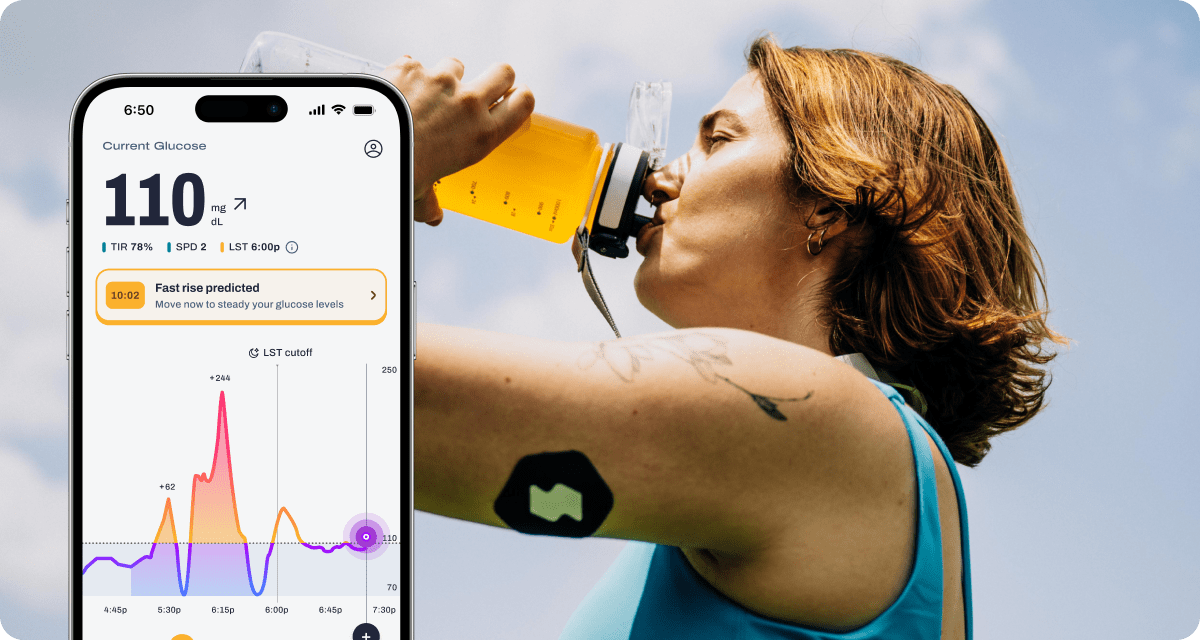
Whether you’re living with prediabetes, managing type 2 diabetes, or simply aiming to better understand your blood sugar patterns, Signos helps you take control of your metabolic health with confidence.
By pairing a continuous glucose monitor (CGM) with advanced AI, Signos gives you real-time feedback on how your body responds to food, movement, stress, and daily habits. This insight helps you spot patterns, make informed decisions, and build sustainable routines that support steadier blood sugar throughout the day.
Signos supports you with:
- Real-time glucose tracking so you can see exactly how your choices influence your blood sugar in the moment.
- Science-backed insights that guide how you eat, move, and recover based on your unique metabolic responses.
- Personalized strategies that adapt to your goals and your starting point, helping you progress at your own pace with clarity and confidence.
With Signos, you’re equipped to understand your body better and make decisions that support long-term metabolic health.
The Bottom Line
Type 1, type 2, and prediabetes may stem from different causes, but one thing is clear: understanding your glucose patterns and taking proactive steps can make a big difference in how you feel and function each day. Whether you’re managing an existing diagnosis or trying to prevent one, consistent monitoring, supportive habits, and practical tools are key.
Learn More With Signos’ Expert Advice
Signos empowers you to take charge of your blood sugar with personalized insights, giving you the confidence to build habits that support your long-term health. Learn more about how Signos can improve your health here, or explore the Signos blog for science-backed tips on managing glucose levels, making lifestyle changes, and supporting your health goals.
Topics discussed in this article:
References
- Understanding Type 1 Diabetes. American Diabetes Association. Accessed November 18, 2025.
- Understanding Type 2 Diabetes. American Diabetes Association. Accessed November 18, 2025.
- Alvarez S, Coffey R, Mathias PM, et al. Prediabetes. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459332/.
- About the Prediabetes Risk Test. Center for Disease Control. Accessed November 18, 2025.



.webp)
.svg)




.webp)





.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
