Key Takeaways
- Poor sleep disrupts cortisol, circadian rhythms, and insulin sensitivity, leading to impaired blood glucose control.
- Sleep loss, even on holiday, increases metabolic stress and drives higher glucose variability.
- Consistent rest and daily routines, supported by Signos insights, can strengthen sleep health and stabilize glucose.
that {{mid-cta}}
The holiday season can feel like a time-less stretch of days: parties that run past midnight, late-night travel, and general festive chaos that pushes past bedtime. And while these nocturnal moments add to the magic of the season, your body is often left to foot the bill.
When you consistently fall short of the 7-8 hours your body needs to stay balanced, sleep debt starts to stack up fast. Even a single night of poor sleep can disrupt key metabolic processes: your cells become more resistant to insulin, cortisol rises, hunger hormones surge, and the glucose patterns that typically keep your energy steady begin to shift.
In this article, we’ll break down what insufficient sleep does to your metabolism, practical ways to recover from it, and how tools like Signos can help you visualize the relationship between sleep and blood sugar to support the right changes.
What Sleep Debt Does to Your Body

Sleep debt is the gap between how much sleep your body needs (7–8 hours) and how much you actually get (we’ll let you fill in that number). During the holidays, late nights with friends and family can easily shave off an hour or two, but even short-term sleep loss can feel like your body has been running on a long-term sleep deficit.
When you don’t get enough sleep, your cells become less responsive to insulin, leaving more glucose circulating in your bloodstream instead of fueling your muscles. In a small study of 16 young men, just one night of about four hours of sleep was enough to reduce insulin sensitivity noticeably, i.e., their metabolism basically protested after one night of poor sleep.
Poor sleep also disrupts your hunger hormones. Ghrelin (the “I’m hungry” hormone) rises, while leptin (the “I’m full” hormone) drops. Throw in a bump in cortisol (the stress hormone) brought on by a lack of sleep, and your brain goes on the hunt for fast energy: sugar, bread, and anything that delivers a quick glucose hit.
The result is a tired body that’s hungrier, less efficient with glucose, and more likely to chase quick sugar.
Cortisol, Circadian Rhythm, and Glucose Control

Whether you’re celebrating late into the night or staying up to watch everyone else do so on Instagram, your circadian rhythm can take a hit. This internal clock regulates your sleep–wake cycle and relies on light cues, such as darkness, to trigger melatonin. Bright lights and late-night screens can disrupt the process, shifting your sleep patterns, delaying the onset of wakefulness, and making it harder for your body to manage glucose. People with sleep apnea, irregular sleep schedules, or shift work often feel these effects even more, since their natural sleep needs are already harder to meet.
Another factor is cortisol; this stress hormone naturally climbs in the early morning to help you rise as part of healthy sleep-wake regulation. But when you’re dealing with sleep loss from holiday fun, poor sleep hygiene, or simply not getting the recommended amount of sleep, cortisol can spike higher than normal. That extra surge triggers glucose spikes, leading to higher morning blood sugar levels.
And if your bedtime swings wildly, 3 AM one night, all tucked in by 10 PM the next, your circadian rhythm struggles to keep up. Even if you’re managing to rest the same number of hours, say six hours every night, irregular rest times make quality sleep harder to achieve, leaving you groggy and dealing with daytime sleepiness. Over time, this disrupted sleep schedule can reduce insulin sensitivity and make glucose control more difficult.
Real-Time Effects You Can See in Glucose Data
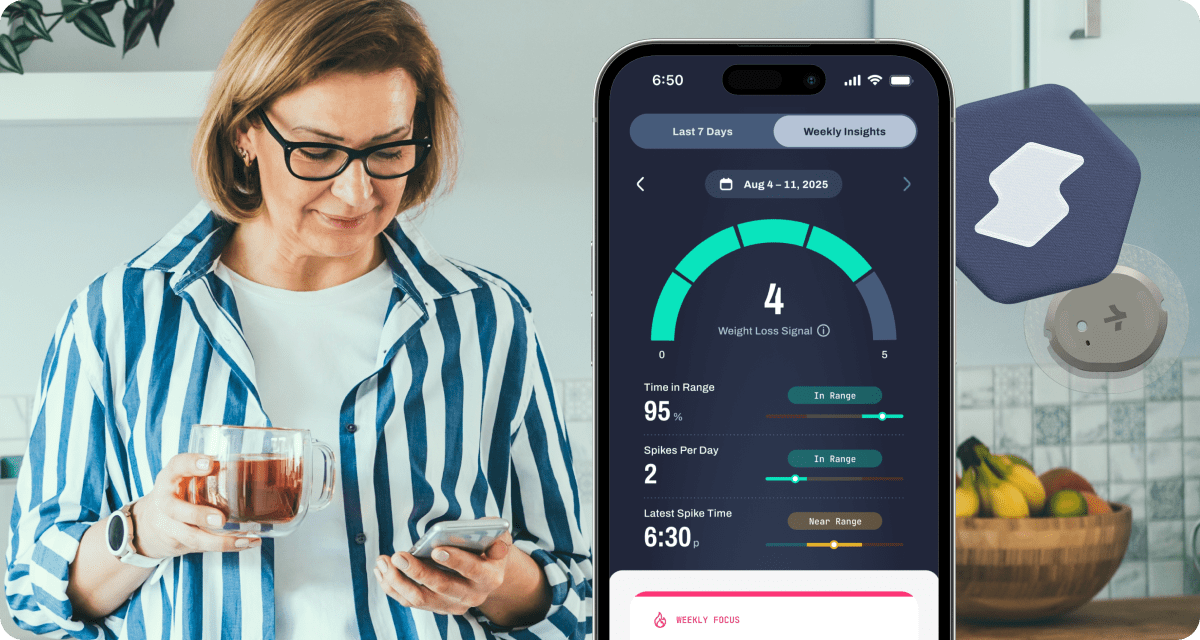
Before you push through next-day grogginess after a night of short or disrupted sleep, it’s worth opening your Signos glucose graph to see what’s happening beneath the surface. Even a single late night often shows up quickly: overnight glucose levels rise, return to baseline more slowly, and become more reactive to habits that commonly follow late nights, like nighttime snacking, alcohol, stress, or scrolling under bright light.
But fatigue isn’t the only side effect. Consistently skimping on sleep or slipping into total sleep deprivation can raise the risk of high blood pressure, impaired insulin sensitivity, weight gain, and metabolic dysfunction. This is why groups like the Sleep Foundation and many healthcare professionals emphasize consistent rest as essential for long-term wellness.
The good news: your body responds quickly to recovery. Even one deep, restorative night can start to steady your glucose and help your system recalibrate. With Signos, you can see this shift in real time: from calmer, more stable overnight readings to smoother daytime glucose patterns. These insights make it easier to understand how sleep quality impacts metabolism and how quickly positive changes pay off.
How to Recover From Sleep Debt

Think of sleep debt recovery as making gradual, repeated deposits, not a single lump-sum payment. If you’ve been dealing with short sleep, disrupted nights, or ongoing sleep deprivation, restoring your rhythm supports better energy, mood, metabolism, and glucose stability.
Start early. Morning sunlight exposure and light movement help realign your circadian rhythm after off-schedule nights. Throughout the day, small adjustments (like a well-timed afternoon nap or a mindful break) can reduce fatigue without derailing your nighttime sleep.
As evening sets in, your habits matter even more. Avoid late-day caffeine, keep dinner on the lighter side, and dial back stimulating activities so your body can transition into sleep more easily. These adjustments help support a healthier next-day glucose response, something you’ll see reflected in your Signos insights.
Experiments to try with Signos:
- Morning Reset Test: Compare your glucose curve on mornings with sunlight and gentle movement vs. mornings without.
- Evening Meal Timing Experiment: Eat dinner 2–3 hours earlier than usual and watch how quickly glucose returns to baseline.
- Screen-Free Hour: Skip bright screens for 60 minutes before bed and observe overnight glucose steadiness.
- Napping Strategy: Try a 10–20 minute nap and compare your afternoon glucose variability on nap vs. no-nap days.
By making these adjustments part of your routine, you gradually reduce the metabolic impact of sleep deprivation and strengthen your overall sleep health.
Building Sleep Resilience Through the Holidays

The holidays bring joy…and chaos. Routines shift, schedules go AWOL, and stress can spike. That’s why building sleep resilience matters: it acts like a buffer, protecting your metabolism and your glucose stability even when life gets unpredictable.
A few consecutive nights of quality sleep can leave you more resilient, reducing the impact of short sleep or late nights that pop up around the holidays. Small habits help, too. A post-dinner walk can lower nighttime glucose, and brief breathwork sessions can quiet stress hormones that interfere with both sleep and glucose stability.
Most importantly, reframing sleep as an active metabolic recovery tool (not a luxury you get when life slows down) can make a meaningful difference. With Signos, you can watch this mindset shift pay off: steadier overnight readings, smoother daytime glucose, and more consistent energy as you move through the holiday season.
Experiments to build holiday sleep resilience:
- Dinner Walk Challenge: Add a 10–15 minute walk after evening meals and compare nighttime glucose levels.
- Stress Downshift Test: Try breathwork or meditation before bed and track overnight glucose stability.
- Consistency Streak: Aim for three nights of regular sleep and look for improvements in glucose variability the following day.
- Late-Night Eating Check: Avoid eating after 8 p.m. for several nights and observe changes in overnight glucose drift.
The Bottom Line
Sleep debt during the holidays won’t just leave you tired; it can disrupt your metabolism and throw your blood sugar off balance. By keeping rest at the top of your itinerary, building steadier routines, and using insights from Signos, you can keep your glucose and energy on track through even the busiest parts of the season.
Learn More With Signos’ Expert Advice
To learn more about building a healthy lifestyle through the holidays and beyond, explore how Signos can help you improve your health through expert guidance. You can also learn more about glucose patterns, sleep, metabolism, and everyday wellness on the Signos blog, where you’ll find clear explanations and practical insights to help you make informed decisions about your health.
Topics discussed in this article:
References
- Briançon-Marjollet, A., Weiszenstein, M., Henri, M., Thomas, A., Godin-Ribuot, D., & Polak, J. (2015). The impact of sleep disorders on glucose metabolism: Endocrine and molecular mechanisms. Diabetology & Metabolic Syndrome, 7, Article 25. https://doi.org/10.1186/s13098-015-0018-3
- Cedernaes, J., Lampola, L., Axelsson, E. K., Liethof, L., Hassanzadeh, S., Yeganeh, A., Broman, J. E., Schiöth, H. B., & Benedict, C. (2016). A single night of partial sleep loss impairs fasting insulin sensitivity but does not affect cephalic phase insulin release in young men. Journal of sleep research, 25(1), 5–10. https://doi.org/10.1111/jsr.12340
- Bryan, L. (2025, July 10). Why do we need sleep? Sleep Foundation. https://www.sleepfoundation.org/how-sleep-works/why-do-we-need-sleep




.svg)










.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
