Many people wake up with elevated blood sugar or higher blood pressure. Even if your numbers look better later in the day, this can feel confusing and even stressful. Morning glucose spikes and blood pressure surges are a common metabolic response. They often are out of our control because your body releases hormones in the early morning to help you wake up and start the day. For some people, these “wake-up” hormones also raise blood glucose and blood pressure more than expected.1
Understanding this pattern is important because repeated morning spikes can strain the cardiovascular system and may make it harder to manage blood sugar throughout the day. By understanding why these changes occur and tracking your personal trends over time, you can take simple steps to support healthier morning patterns and your metabolic health.
What Causes Morning Blood Sugar Spikes?
.png)
Many people notice higher blood sugar in the morning, even if they didn’t eat overnight. This pattern is often called “Dawn Phenomenon". It happens because your body naturally releases a cascade of hormones in the early morning hours to help you naturally feel awake and get moving. These hormones include cortisol, growth hormone, and adrenaline. And they start spiking before you’ve woken up for the day.1
While helpful for that natural boost of morning energy, these hormones also tell your liver to release stored glucose into your bloodstream. Thus, you might notice that your morning numbers are slightly elevated. This is especially true if you have insulin resistance, as blood sugar can rise more than expected in the early morning hours. For people with insulin resistance or type 2 diabetes, this effect is often stronger.2
If you’re on medication to manage your blood sugar, some diabetes medications wear off overnight or may not fully cover early morning hormone surges. Plus, steroids, certain blood pressure medications, and late-night snacks combined with medication timing can also affect fasting glucose levels. Adjusting your timing or dose with a healthcare provider can sometimes improve morning surges.
Lastly, chronic stress and disrupted sleep raise cortisol levels even further. In turn, this can exacerbate morning glucose spikes and increase day-to-day glucose variability. Learning to manage your stress and improving sleep quality often helps smooth out these early-day rises.
What About High Blood Pressure in the Mornings?
.jpg)
Similar to your blood sugar, the early-morning surge of hormones also affects blood pressure. Blood pressure naturally follows a daily rhythm called the circadian pattern. During sleep, blood pressure usually drops lower. In the early morning, it rises again as your body prepares to wake up. This is known as the morning blood pressure surge. For some people, this rise is mild. For others, it can be much stronger and show up as high blood pressure in the morning.3
Cortisol is a stress hormone well-known for increasing alertness and energy, but it also affects blood pressure. Higher morning cortisol levels cause blood vessels to constrict slightly and increase the amount of sodium the body retains. Together, these effects raise blood pressure. If cortisol levels stay elevated due to stress, poor sleep, or chronic inflammation, morning blood pressure can spike higher than your usual baseline.4
Plus, as you wake up, your “fight or flight” nervous system becomes active. This is a natural response to waking up that increases heart rate and blood vessel tone, thereby pushing blood pressure upward. In folks with insulin resistance, obesity, or existing high blood pressure, this response is often exaggerated.
Understanding the Metabolic Link between Morning Hypertension and Blood Sugar
Morning blood sugar spikes and morning hypertension often co-occur because they are driven by many of the same biological signals. Their biggest shared factor is stress hormones, particularly cortisol and adrenaline. These hormones rise naturally in the early morning to help you wake up. In doing so, they increase glucose release from the liver and cause blood vessels to tighten, which raises both blood sugar and blood pressure.
In metabolically healthy folks, this natural morning response isn’t significant enough to warrant concern. However, there are a few factors that exacerbate the Dawn Phenomenon effects:
- Insulin resistance: When cells don’t respond well to insulin, glucose stays in the bloodstream longer. This makes the liver’s early-morning glucose release harder to control, leading to larger fasting glucose spikes. Research shows that poorer glucose control is associated with larger morning blood pressure surges, especially in people with metabolic conditions.5
- Stress and anxiety: Chronic stress elevates cortisol levels. Higher cortisol levels increase glucose production and promote blood vessel constriction, which can raise both blood sugar and blood pressure in the morning.4
- Pre-existing conditions like diabetes and hypertension: If blood sugar or blood pressure regulation is already impaired, the body has less ability to buffer morning hormone surges. This may exaggerate morning spikes or make it more difficult to manage them with diet and exercise alone.
- Nighttime snacking: Late eating, especially of high-carb or high-sugar foods, can raise overnight glucose levels and disrupt normal insulin patterns. This can worsen fasting glucose spikes the next morning.2
- Poor sleep habits: Short or disrupted sleep raises stress hormones and reduces insulin sensitivity. This combination makes it more likely that blood sugar and blood pressure will rise when you wake up.6
- Sedentary lifestyle: Low daily movement reduces insulin sensitivity and cardiovascular fitness. This makes it harder for the body to manage glucose efficiently and regulate blood vessel function.7
Long-Term Risks and Health Side Effects
Repeated morning surges in blood pressure and blood sugar place extra strain on the heart and blood vessels. Over time, this pattern is linked to metabolic risk factors. That’s why noticing consistent morning spikes is important, even if your readings improve later in the day.
Here are the most prevalent risks associated with high morning blood sugar surges or elevated blood pressure levels:
- Cardiovascular strain: When blood pressure rises sharply in the morning, the heart and blood vessels experience higher pressure during a vulnerable time of day. Research shows that large morning blood pressure surges are linked to a higher risk of heart attack, stroke, and blood vessel damage. Plus, over time, this added strain can contribute to stiff arteries and reduced blood vessel flexibility.8,9
- Worsening insulin resistance: Frequent fasting glucose spikes indicate the body is struggling to regulate blood sugar effectively. When this pattern continues, it can reinforce insulin resistance, making it harder for cells to respond to insulin and increasing the risk of type 2 diabetes and metabolic dysfunction.10
- Long-term metabolic risk: When high morning glucose and high blood pressure co-occur, they may reflect broader metabolic stress. Over time, this can increase the risk of cardiometabolic conditions, including hypertension, diabetes, and abnormal cholesterol patterns.11
How to Monitor
.png)
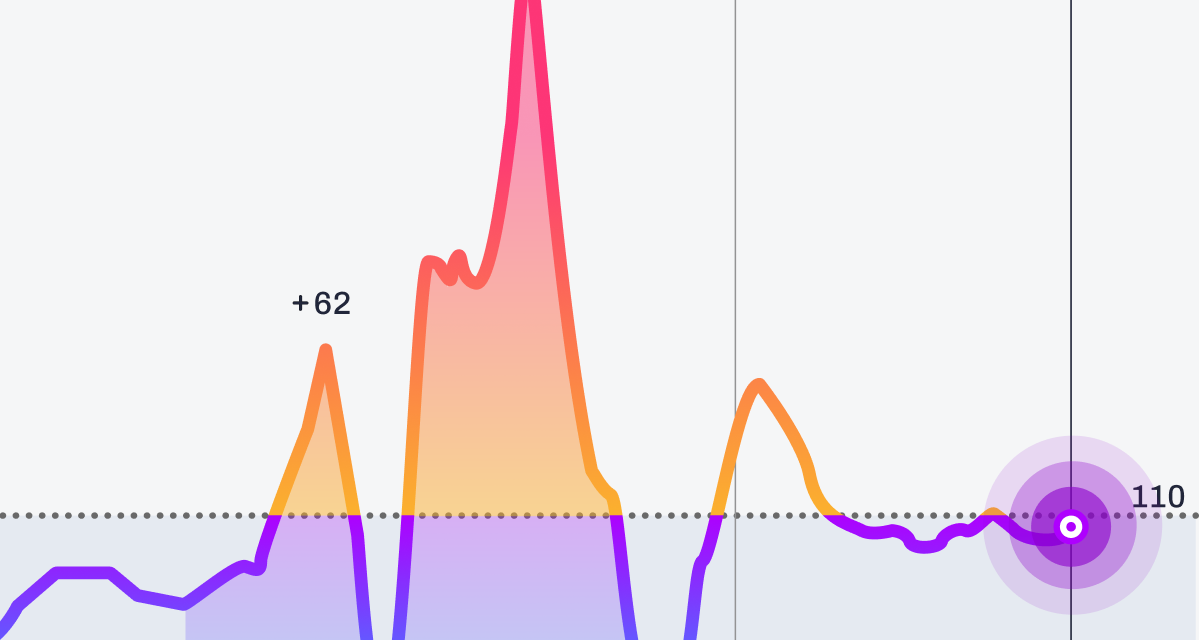
Tracking patterns over time can help you better understand what your body is doing in the morning. While these tools are not diagnostic, they can provide helpful insight into trends that may reflect metabolic stress, sleep quality, stress levels, and lifestyle habits.
- Continuous glucose monitors (CGMs): CGMs show how blood sugar changes throughout the day and overnight. This makes it easier to spot fasting glucose spikes, early morning rises related to the dawn phenomenon, and how meals, sleep, and activity affect glucose variability. Instead of focusing on single numbers, the goal is to look for repeated patterns.
- Home blood pressure cuffs: Checking blood pressure in the morning at the same time each day can reveal whether you experience a consistent morning blood pressure surge. Tracking trends over several days or weeks provides more useful information than one isolated reading.
Remember, daily measurements can fluctuate for many reasons, including stress, poor sleep, or dehydration. It is your trend or pattern over time that offers the best insight into how your body responds to daily habits and recovery.
What You Can Do
.png)
Small, consistent changes can make a meaningful difference in both morning glucose spikes and blood pressure surges. The goal is not perfection, but supporting your body’s natural rhythms.
- Prioritize sleep quality: Aim for consistent bed and wake times to support circadian rhythm regulation, which influences cortisol, insulin sensitivity, and morning blood sugar.
- Eat balanced evening meals: Include protein, fiber, and healthy fats at dinner to help stabilize overnight glucose levels and reduce large morning spikes.
- Avoid late-night heavy snacking: Eating large, high-carb meals close to bedtime can raise fasting glucose the next morning.
- Stay hydrated: Dehydration can contribute to higher morning blood pressure and thicker blood volume. Drinking water consistently throughout the day supports better morning readings.
- Incorporate regular physical activity: Daily movement improves insulin sensitivity and helps regulate blood pressure. Even light evening walks can support overnight glucose stability.
- Manage stress before bed: Relaxation strategies such as breathing exercises, stretching, or limiting screen time can help reduce nighttime cortisol release.
- Review medications with your healthcare provider: Some blood pressure, diabetes, or steroid medications affect morning readings. Your provider may adjust timing or dosing if patterns persist.
- Maintain consistent morning routines: Checking glucose or blood pressure at the same time each day creates more reliable trend data and reduces measurement variability.
How Signos Can Help
.png)
Signos helps turn awareness into action by revealing your personal morning glucose trends and daily patterns, and showing you exactly what to test next. With real-time glucose data from a continuous glucose monitor and guided in-app Experiments, you can see how small, intentional changes affect your body in real life.
Members can try simple experiments such as:
- Protein-first breakfast: Eat protein and fiber before carbohydrates and observe how your morning glucose response changes.
- Post-meal movement: Take a 10–15 minute walk after meals to see how light movement influences glucose spikes.
- Earlier dinner timing: Finish dinner earlier in the evening and track overnight stability and morning glucose trends.
- Sleep consistency: Compare glucose variability on well-rested days versus nights with shorter or disrupted sleep.
- Stress awareness: Notice how high-stress mornings or rushed meals affect glucose compared to calmer routines.
The Signos app connects these experiments to Insights, Dailies, and Badges, helping you see progress through habit consistency, not just long-term outcomes. Over time, these repeatable experiments reveal what works best for your body and help reinforce proactive habits that support metabolic health, energy, and sustainable progress.
Topics discussed in this article:
References
- O'Neal TB, Luther EE. Dawn Phenomenon. [Updated 2023 May 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan.
- High Morning Blood Glucose: Understanding and Management. American Heart Association. Accessed January 19, 2026.
- Gosse P, Schumacher H. Early morning blood pressure surge. J Clin Hypertens (Greenwich). 2006;8(8):584-589. doi:10.1111/j.1524-6175.2006.04773.x
- Kaur J, Gandhi J, Sharma S. Physiology, Cortisol. [Updated 2025 Dec 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan.
- Koichiro Yoda, Masaaki Inaba, Kae Hamamoto, Maki Yoda, Akihiro Tsuda, Katsuhito Mori, Shinsuke Yamada, Masanori Emoto, Hidenori Koyama, Yasuo Imanishi; Association Between Glycemic Control and Morning Blood Pressure Surge With Vascular Endothelial Dysfunction in Type 2 Diabetic Patients. Diabetes Care 1 March 2014; 37 (3): 644–650.
- Yano Y, Gao Y, Johnson DA, et al. Sleep Characteristics and Measures of Glucose Metabolism in Blacks: The Jackson Heart Study. J Am Heart Assoc. 2020;9(9):e013209. doi:10.1161/JAHA.119.013209
- Dimitriadis GD, Chryssanthopoulos C, Philippou A, Koutsilieris M. The Significant Role of Physical Activity and Exercise in Health and Metabolic Diseases. Physiologia. 2025; 5(4):57. https://doi.org/10.3390/physiologia5040057
- White WB. The risk of waking-up: impact of the morning surge in blood pressure. Hypertension. 2010;55(4):835-837. doi:10.1161/HYPERTENSIONAHA.109.148908
- Poznyak AV, Litvinova L, Poggio P, Sukhorukov VN, Orekhov AN. Effect of Glucose Levels on Cardiovascular Risk. Cells. 2022;11(19):3034. Published 2022 Sep 28. doi:10.3390/cells11193034
- Freeman AM, Acevedo LA, Pennings N. Insulin Resistance. [Updated 2023 Aug 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan.
- Petrie JR, Guzik TJ, Touyz RM. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Can J Cardiol. 2018;34(5):575-584. doi:10.1016/j.cjca.2017.12.005


.webp)
.svg)










.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
