Key Takeaways
- Most people with PCOS experience some degree of insulin resistance, regardless of body weight or appearance.
- Poor blood sugar control worsens hormone imbalance, inflammation, energy crashes, cravings, and long-term cardiometabolic risk.
- Nutrition is a powerful tool for managing PCOS symptoms when it prioritizes glucose stability rather than restriction.
- Learning how foods influence insulin and blood sugar after meals can guide healthier eating choices.
that {{mid-cta}}
Polycystic ovary syndrome (PCOS) is not only a reproductive condition; it is, for many people, a metabolic condition caused by insulin resistance and impaired blood sugar regulation.1 Research consistently proves that people with PCOS experience some degree of insulin resistance, regardless of body weight or appearance.
This metabolic disruption affects hormone signaling, ovarian function, inflammation, energy levels, and can lead to long-term cardiometabolic risks.
Since insulin plays such a big role in PCOS, nutrition becomes one of the biggest and most influential tools for symptom management. However, many people get vague and often contradictory advice, such as “cut carbs,” “eat low-GI,” and “try anti-inflammatory foods," all without a clear explanation as to why they should do that or how to implement them into their lifestyle.
This article focuses on PCOS nutrition through the lens of blood sugar control. We will explain how specific foods and dietary patterns can influence insulin sensitivity, post-meal glucose levels, and even metabolic stability.
Understanding the Link Between PCOS, Insulin Resistance, and Blood Sugar
.jpg)
Before we talk about specific foods, it is important to understand the metabolic foundation of PCOS.
In insulin resistance, cells do not respond efficiently to insulin’s signal to absorb glucose from the bloodstream. The pancreas tries to compensate by producing more insulin, which leads to elevated insulin levels.
This elevated insulin level then stimulates excess androgen production in the ovaries, worsens ovulatory dysfunction, and promotes fat storage, specifically visceral fat, which further increases insulin resistance.2
This means that PCOS nutrition strategies must prioritize blood sugar stability, insulin sensitivity, and metabolic resilience rather than restricting calories or imposing rigid food rules.
Post-Meal Sugar Spikes After “Normal” Meals
.jpg)
Many individuals with PCOS experience highly elevated blood sugar spikes after meals that wouldn’t affect someone without insulin resistance. Even meals that look "healthy," such as oatmeal, smoothies, or whole-grain toast, can trigger rapid glucose spikes followed by an energy crash.
Consistent post-meal glucose spikes drive higher insulin secretion. Over an extended period of time, this worsens insulin resistance, disrupts appetite regulation, increases fat storage, and intensifies PCOS symptoms like irregular cycles, fatigue, and acne.
Low Glycemic, Fiber-Rich Carbohydrates
Effective PCOS nutrition does not eliminate carbohydrates; instead, it optimizes carbohydrate quality.
Foods that support a stable post-meal glucose are:
- Lentils, chickpeas, and black beans.
- Steel-cut oats instead of instant oats.
- Quinoa, farro, and barley
- Non-starchy vegetables, like leafy greens, broccoli, zucchini, and cauliflower.
These foods take longer to digest, slow glucose absorption, and improve insulin sensitivity due to the higher levels of fiber ingested. Fiber also promotes good gut health, which in turn improves your metabolic health as well.
High Carbohydrate Sensitivity and Glucose Variability
.jpg)
People with PCOS often feel unwell after eating a carb-heavy meal, even when the total calorie amount is reasonable. Symptoms generally include fatigue, brain fog, cravings, and, in some cases, mood changes.
Carbohydrate sensitivity indicates impaired glucose handling rather than carbohydrate intolerance. Large or poorly balanced carb loads can increase insulin demand, promote fat storage, and disrupt hunger hormones, which makes long-term diet consistency nearly impossible.
Strategic Carbohydrate Pairing
One of the best and most effective ways to address this is through a PCOS nutrition strategy called food pairing.
Carbohydrates should almost always be paired with these foods:
- Lean protein (eggs, fish, chicken, Greek yogurt, tofu).
- Healthy fats (olive oil, avocado, nuts, and seeds).
- Vegetables rich in fiber.
For example, pairing fruit with protein and fat, rather than eating it alone, can drastically reduce glucose spikes after the meal. This approach improves metabolic control without forcing you to eliminate carbs at all.
Chronic Low-Grade Inflammation
PCOS is often associated with low-grade inflammation driven by insulin resistance, oxidative stress, and visceral fat accumulation.
This inflammation worsens insulin resistance and directly interferes with normal ovarian signaling. In some cases, it can also be associated with increased cardiovascular risk and fatigue.
Anti-Inflammatory Foods That Improve Insulin Sensitivity
PCOS nutrition should include foods with anti-inflammatory and insulin-sensitizing properties, such as:
- Fatty fish rich in omega-3s, such as salmon, sardines, and mackerel.
- Extra-virgin olive oil.
- Walnuts, flaxseeds, and chia seeds.
- Colorful vegetables and berries rich in polyphenols.
These foods help reduce inflammation while also improving cellular insulin responses over time.
Confusion Around “Healthy” Foods
.jpg)
People with PCOS are usually told to simply eat “healthy,” but foods marketed as healthy, such as granola, smoothies, and plant-based baked goods, often contain a concentrated amount of carbohydrates that can destabilize blood sugar.
When “healthy” foods repeatedly trigger blood sugar spikes, insulin levels rise sharply. Over time, this can reinforce insulin resistance, worsen androgen excess, and even increase glucose variability. A lot of people with PCOS try to counteract this by further restricting food or feeling confused about why the symptoms persist and get worse despite eating “healthy.”
This mismatch between what seems to be healthfulness and metabolic response undermines confidence in nutrition strategies and can delay meaningful improvements in blood sugar control.
Choose Foods with Intact Structure and Predictable Glycemic Response
Effective PCOS nutrition prioritizes how a food behaves in the body, not how it is marketed. Foods with an intact fiber structure are digested much more slowly, produce smaller glucose excursions, and require less insulin.
Here are some popular foods and their ideal swaps for PCOS blood sugar control:
- Whole fruit instead of fruit juice or smoothies.
- Plain Greek yogurt with berries instead of flavored yogurt.
- Steel-cut oats over instant oats and granola.
- Whole legumes over a legume-based snack product.
- Homemade meals instead of a packaged “health” bar.
Another important strategy to consider is reducing liquid carbohydrates, which bypass normal digestion and lead to higher glucose absorption. Smoothies, juices, and sweetened beverages, even the ones made with whole ingredients, often produce higher glucose spikes than eating the same foods whole.
By focusing on minimally processed foods with intact fibers, PCOS nutrition becomes much more sustainable, predictable, and metabolically supportive.
Energy Crashes and Blood Sugar Lows Between Meals
.jpg)
Energy crashes one to three hours after eating are a common issue that people with PCOS experience daily. These crashes generally occur mid-morning or mid-afternoon and are mistaken for caffeine dependency, stress, or lack of sleep. But in reality, they are frequently caused by a drastic drop in blood sugar after an insulin spike.
Meals that are low in protein, fiber, or fat, such as cereal, snack bars, and smoothies, will digest quickly, triggering a rapid glucose rise followed by a strong crash.
Blood sugar lows increase hunger hormones and cravings, especially for carbs. If left unchecked, this pattern reinforces glucose variability, worsens insulin resistance, and makes appetite regulation very difficult.
Not to mention that energy instability can also affect your concentration, exercise consistency, and overall mood, all of which indirectly influence your PCOS symptom management.5
High-Protein Meals with Blood Sugar-Stabilizing Foods
For PCOS blood sugar control, protein is non-negotiable in every meal. Protein reduces post-meal glucose spikes and provides a steadier energy release.
The best protein-rich foods for PCOS nutrition include:
- Eggs and egg whites.
- Fish (salmon, tuna, sardines).
- Chicken and turkey.
- Greek yogurt and cottage cheese.
- Tofu, tempeh, and edamame.
A protein-forward meal is one of the most reliable ways to reduce energy crashes and improve daily blood sugar stability.
Elevated Insulin Driving Androgen Excess
In PCOS, insulin does a lot more than regulate blood sugar. It is directly involved in stimulating the ovaries to produce androgens. When insulin levels remain chronically elevated due to consistent glucose spikes, androgen production increases even further.
Excess androgens contribute to symptoms such as acne, hair thinning, irregular ovulation, and struggling to maintain metabolic balance. After a while, hyperinsulinemia can worsen reproductive dysfunction and increase cardiometabolic risk.
Foods That Lower Insulin on Demand
Lowering your insulin levels does not require you to remove carbs from your meals; instead, it requires meals that help you consistently reduce insulin levels.
Food that can lower insulin response includes:
- Healthy fats (olive oil, seeds, and nuts).
- Low-glycemic carbs (chickpeas, lentils, and quinoa).
- Non-starchy vegetables (spinach, kale, and asparagus).
These foods form the core of a solid PCOS nutrition plan and will decrease insulin secretion, which can indirectly reduce androgen signaling and support hormonal balance over time.
Poor Gut Health Contributing to Blood Sugar Dysregulation
Research shows that many individuals with PCOS have altered gut microbiome composition.3 Low fiber intake, chronic inflammation, and frequent blood sugar swings can disrupt gut barrier integrity and microbial diversity.
Poor gut health can increase systemic inflammation and worsen insulin resistance.4 It can also make it harder for your body to fully absorb nutrients, all while amplifying glucose variability. This all makes blood sugar control more difficult, even with dietary changes.
Gut-Supporting Foods That Improve Glucose Regulation
The best foods for PCOS blood sugar control tend to overlap with foods recommended for gut health.
Key gut-supportive foods include:
- Fermented foods, such as yogurt, kefir, kimchi, and sauerkraut.
- Prebiotic-rich vegetables, like onions, garlic, leeks, and asparagus.
- Legumes and whole grains that provide fermentable fiber.
Incorporating these foods into PCOS nutrition strategies will help regulate blood sugar through metabolic and gut-mediated pathways.
Avoidance of Dietary Fat Leading to Glucose Instability
.jpg)
Some individuals with PCOS still follow a low to no-fat diet due to outdated dietary advice or fear of weight gain. This tends to result in meals mainly composed of carbs, with little to no fat or protein, such as cereal, toast, and rice bowls. While these meals may appear healthy, they often lack the macronutrient balance necessary for stable blood sugar regulation.
For people with PCOS, avoiding fat is problematic because insulin resistance is already accelerating glucose absorption. So, without dietary fat to slow digestion down, carbs enter the bloodstream rapidly, triggering larger glucose spikes.
Low-fat meals digest quickly, leading to faster glucose absorption and larger insulin spikes. They are also the cause of reduced satiety, which increases the odds of overeating later in the day.
From a hormonal perspective, elevated insulin can increase ovarian androgen production, which can directly intensify symptoms such as acne, hair changes, and irregular cycles.6 This all means that avoiding fat can worsen both the metabolic and hormonal aspects of PCOS.
Use Healthy Fats as a Blood Sugar-Stabilizing Tool
In PCOS nutrition, dietary fat is the stabilizer needed in most meals. The best fat sources for PCOS blood sugar control are these:
- Avocado and avocado oil.
- Almonds, walnuts, pistachios, and pecans.
- Chia, flax, pumpkin, and sunflower seeds.
- Mackerel, sardines, and salmon.
- Extra virgin olive oil.
Practical use of fats means adding them to your meals intentionally, not excessively. For example, pairing a salad with olive oil and chicken produces a smaller glucose response than eating the salad alone.
When used strategically, healthy fats make PCOS nutrition sustainable and stable.
Over-Restriction Creates Metabolic and Hormonal Stress
.jpg)
When trying to control weight or symptoms, many people with PCOS adopt very restrictive diets. These diets tend to remove carbs entirely, skip meals, or reduce their caloric intake to a minimum. Not only are these diets outdated and unhealthy, but they can also increase the likelihood of overeating, which further increases glucose spikes and emotional distress when it comes to food.
Long-term restrictions can also disrupt hunger and satiety cues, making it hard to recognize what the body truly needs. Instead of improving your metabolic health, this diet often worsens your insulin resistance and contributes to diet fatigue and burnout.
Build Sustainable Eating Patterns Around Blood Sugar Stability
Effective PCOS nutrition isn’t about eating less, but about eating strategically. Meals should be balanced and built around foods that can naturally stabilize blood sugar.
A sustainable pattern for PCOS blood sugar control should include:
- Including protein, fiber, and fat in every meal.
- Eating consistent meals throughout the day.
- Choosing carbs for glycemic impact rather than removing them.
- Being flexible to reduce stress.
When meals are structured to support blood sugar stability, hunger becomes more predictable, cravings go down, and insulin sensitivity improves over time. This approach supports long-term metabolic health without the physiological stress associated with restrictive dieting.
Why Adding Foods Matters More Than Cutting Them in PCOS
The ideal and most effective PCOS nutrition strategy is not a restrictive diet but a food-based framework focused on stabilizing blood sugar. Choosing foods that slow digestion, reduce insulin on demand, and support metabolic health allows people with PCOS to handle symptoms without sacrificing their health in the process.
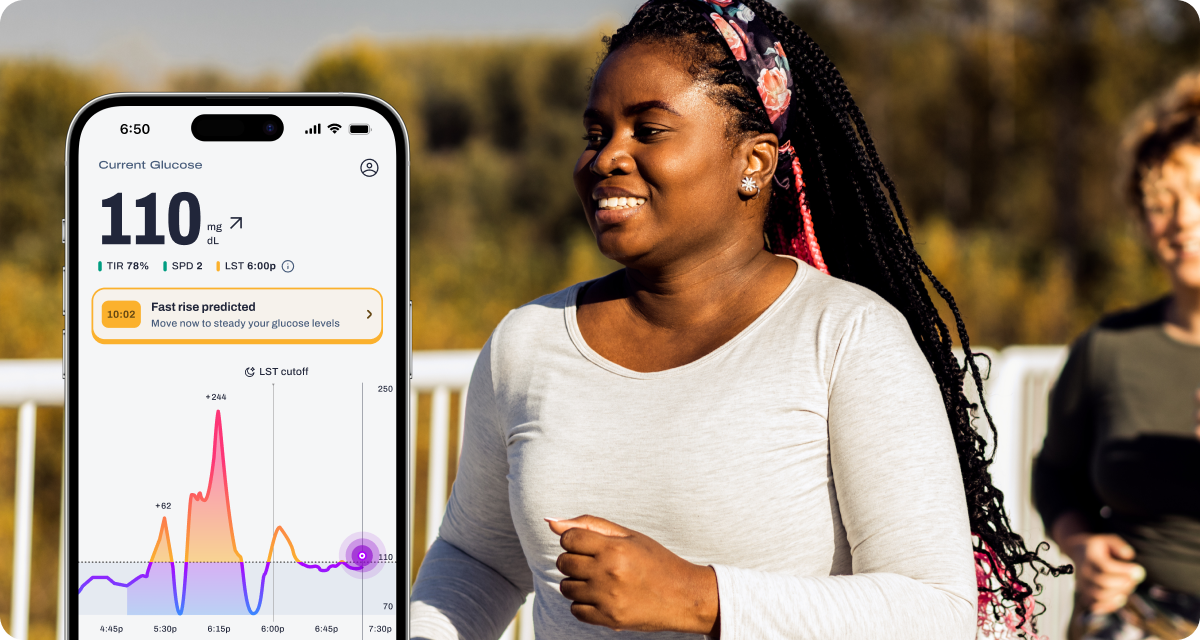
Learn More With Signos’ Expert Advice
If you want to understand better how your daily habits influence your metabolic health, Signos offers expert-backed education and tools to help you build healthier routines. You can explore how glucose patterns connect to energy, hunger, and your overall well-being, and learn more about glucose levels through Signos’ blog.
Topics discussed in this article:
References
1. Cleveland Clinic. (n.d.). Polycystic ovary syndrome (PCOS). https://my.clevelandclinic.org/health/diseases/8316-polycystic-ovary-syndrome-pcos
2. Escobar-Morreale, H. F. (2018). Polycystic ovary syndrome: Definition, aetiology, diagnosis and treatment. Nature Reviews Endocrinology, 14(5), 270–284. https://pmc.ncbi.nlm.nih.gov/articles/PMC9665922/
3. Franks, S., Stark, J., & Hardy, K. (2008). Follicle dynamics and anovulation in polycystic ovary syndrome. Human Reproduction Update, 14(4), 367–378. https://pmc.ncbi.nlm.nih.gov/articles/PMC9998696/
4. Johns Hopkins Medicine. (n.d.). Your digestive system: 5 ways to support gut health. https://www.hopkinsmedicine.org/health/wellness-and-prevention/your-digestive-system-5-ways-to-support-gut-health
5. NHS. (n.d.). Polycystic ovary syndrome (PCOS) – Symptoms. https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/symptoms/
6. Rizk, M. G., & Thackray, V. G. (2021). Intersection of polycystic ovary syndrome and the gut microbiome. Journal of Endocrinology, 249(2), R43–R59. https://pmc.ncbi.nlm.nih.gov/articles/PMC8107978/


%20(1).jpg)

.svg)










.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
